Introduction

Source: https://thehimalayantimes.com/opinion/altitude-sickness-dos-donts (Ratna Sagar Shrestha/THT)
Traveling to high-altitude places is becoming increasingly ever-so-popular, especially for outdoor lovers and adventure seekers. In Nepal, home to eight of the 14 tallest mountains in the world, the Department of Tourism issued a record-breaking 408 permits to climb Mt. Everest alone, and many more issued to summit the other extreme altitude mountains throughout the country. The demand for these adventures was so high, it began to become unfeasible for conservation, and scale backs were put for in place for 2022 and beyond.
This is just in Nepal also, as there are many other places across the globe that are seeing an increase in tourism. Over the past 10 years (excluding 2021 due to COVID restrictions), Mount Denali in Alaska has seen an increase in summits by 9% annually. With an increase in travel to these places, it is important to understand the risk factors involved and take adequate steps to prepare.
For those with little mountaineering experience, traveling to places with high altitudes can be a serious health threat. Not only do mountains possess geological risks of rock-slides, avalanches, and unpredictable weather events, but they can also create adverse health effects on the body once ascended past certain altitudes. One of these affects the lungs directly, which causes fluid to accumulate inside and has life-threatening consequences.
What is HAPE?
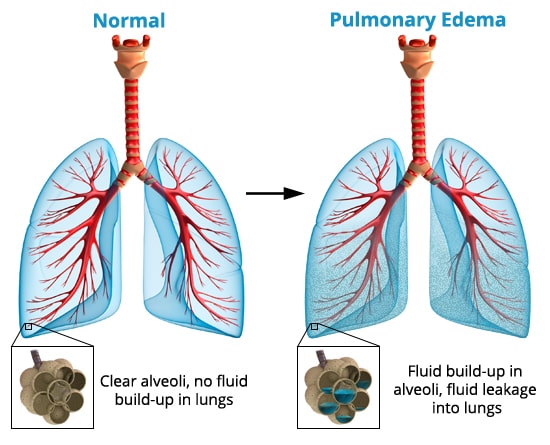
The accumulation of abnormal fluid in the lungs is classified medically as pulmonary edema. When pulmonary edema occurs in high altitudes, it is further classified as High Altitude Pulmonary Edema (HAPE). Although the fluid build-up in the lungs is similar, HAPE is more nuanced in the way it occurs. The causes for Pulmonary Edema vary, but ordinarily, it is from a cardiovascular issue, with increased heart pressure pushing fluid into the lungs. In HAPE, hypoxia (lack of oxygen) causes a breakdown in the pulmonary blood-gas barrier, which leads to leakage of plasma and even red blood cells in the lung.
HAPE can occur at ascensions above 8,200 ft. of elevation, but the risks increase with further increases of elevation. The symptoms will start off with a subtle cough, shortness of breath with exertion, and difficulty walking uphill. These are also signs of Acute Mountain Sickness (AMS), which makes an initial diagnosis difficult. As it progresses though, coughing and difficulty breathing will become more intense and even light exercise will require much more exertion. The cough can produce a pink, frothy mucus and can also contain heavier concentrations of blood. These symptoms, along with prolonged hypoxia can be life-threatening without proper descent. In some cases, this can lead to another severe form of altitude sickness, High Altitude Cerebral Edema (HACE), where a similar process occurs in the brain.
Treatment & Prevention

Luckily, HAPE has little reluctance to hang around when descending to lower elevations. The most recommended is to turn back and head to an elevation plentiful in oxygen, use supplemental oxygen, or both. In occasions where this is not possible, tadalafil or sildenafil can be given to reduce pulmonary pressure, although this isn’t a standard that most mountaineers swear by. In moderate to severe cases, HAPE requires additional evaluation and treatment once reaching low elevation by medical professionals.
Preventing HAPE can be tricky, but the important guidelines are a slow ascent of 300 to 350 m (approximately 1,000 to 1,200 ft.) per day along with an extra acclimatization day added for every 600 to 1,200 m (approximately 2,000 to 4,000 ft) above 2,500 m (approximately 8,200 ft.). Dexamethasone, a common treatment for acute mountain sickness, has also been used as a preventative measure for HAPE, although larger studies are required to confirm the role of this drug in the prevention of HAPE.