Altitude Sickness is an all-too-common affliction for mountain newcomers and is always on the radar for even the most veteran mountain-enjoyers. As one increases in altitude, the surrounding air pressure decreases as less air is pushing down from above. Despite common misconceptions, there is no ‘less oxygen’ at higher altitudes — the oxygen content of air hovers around 21% throughout the entire atmosphere[1] — rather, the lower air pressure is the cause of decreased oxygen intake for anybody visiting the mountains. Each breath literally brings in less air and only by proxy brings in less oxygen. It is this decreased oxygen intake that causes the symptoms of Altitude Sickness, also called Acute Mountain Sickness (AMS), which usually affects first-time visitors far more severely than those more familiar with being at altitude.
Common Altitude Sickness
AMS is the result of decreased blood oxygen saturation, and affects between 10% and 20% of experienced hikers, climbers, skiers, and general mountaineers, but affects as many as 70% or 80% of first-time mountain goers. The symptoms of AMS usually begin within 24 hours at elevations at or above 2,500m (8,000ft) but can occur in more sensitive individuals as low as 1,500m (5,000ft). Symptoms are often mild, including headache, nausea, and fatigue, nothing more than a bad hangover, but the severity of these symptoms tends to increase with elevation as the air becomes thinner and less oxygen dense with every extra foot. A sustained lack of oxygen to the brain is known as hypoxia, which results in lesser brain function, and confusion, and in severe cases, can induce coma and even death [2]. AMS and hypoxia, being the result of oxygen deprivation, can easily be treated with supplemental oxygen, including Boost Oxygen™, a convenient and portable oxygen supply allowing better performance for high-altitude athletes.

Severe Cases and Complications
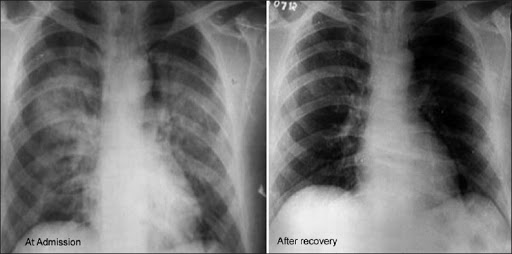
There are, however, complications of AMS that can be fatal if left untreated. High Altitude Pulmonary Edema (HAPE) and Cerebral Edema (HACE) are the direct results of the low air pressure found at high elevations, both of which are made worse by sustained hypoxia. An Edema is an excess of fluid; Pulmonary meaning in the lungs and Cerebral meaning in the brain. A body that is not acclimated to lower air pressure will develop high blood pressure, or hypertension, which can rupture the alveoli, the tiny air sacs in the lungs which facilitate respiration. This excess fluid can worsen the symptoms of hypoxia and can be fatal [3]. Cerebral Edema causes an increase in intracranial pressure (the pressure within the skull), reducing brain function further, which can also be fatal [4].
The dangers of HAPE and HACE are not only found in their symptoms, however. Many novice and experienced mountaineers confuse the symptoms of HAPE and HACE with AMS and overlook the severity of their underlying condition. HAPE and HACE cannot be treated with supplemental oxygen alone and thus require immediate descent and acute medical intervention. It is for this reason that HAPE and HACE can be so dangerous; their symptoms are often left untreated because they are confused with those of AMS and those afflicted won’t always seek immediate medical attention [5].
The most common cause of high altitude death is Pulmonary and Cerebral Edema-induced hypoxia and the only surefire way to identify Pulmonary or Cerebral Edema is by lung and brain scans, so if you notice any of the following symptoms on your next high altitude excursion, don’t take any chances, and descend immediately.
Prevent and Identify
The safest way to treat AMS, HAPE, and HACE, is to avoid having to treat them at all. Altitude Acclimation is the best way to prevent AMS or its complications from developing in both novice and veteran mountaineers. It is recommended that you stop for multiple hours about halfway to your final elevation, or that you rest at elevation for 24 hours before hiking, skiing, or climbing above 8,000ft. Additionally, carb-loading and creatine are great dietary methods to increase oxygen uptake before making an ascent [6]. Unfortunately, this means that high-altitude day trips may be off the table but at least you now have a reason to eat lots of pasta.
If prevention isn’t feasible, the best solution is being able to accurately identify and differentiate between AMS, HAPE, and HACE. AMS is the precursor to pulmonary and cerebral edemas, so if you notice the onset of AMS symptoms after a rapid ascent, be on the lookout for more severe symptoms. Those more severe symptoms include confusion and disorientation (HACE) as well as a persistent dry cough which may develop into a bloody or mucus-filled cough (HAPE) [7]. If either of these symptoms develops, remember to descend immediately and seek medical care.
So What?
As a person who has only once experienced the serious effects of Altitude Sickness, it’s rarely ever on my mind. That’s what you, the reader may be thinking as well; if I’ve never experienced this before, why should I be concerned? The answer to this question is two-fold.
In an airplane, the flight attendants will always tell you to ‘put your mask on before assisting others’. This is because if you pass out from hypoxia in an airplane, you won’t be able to help period, so your own safety goes first. This reasoning extends to the hypoxia symptoms you may notice in your riding partners. Once the onset of hypoxia begins, their ability to make the decision to descend will decrease so the decision to descend may be up to you, even if you’re not experiencing the same symptoms. You, in effect, may become responsible for their decision-making if the onset is rapid enough. Even those who aren’t as susceptible to AMS may still find this information valuable and potentially lifesaving.
Additionally, repeat or prolonged hypoxia may result in permanent brain damage. The effects of untreated hypoxia are fatal, a fact which has been explained at length thus far. But if hypoxia remains untreated for an extended period of time, the effects could last a lifetime.

It’s Real
I myself have experienced AMS symptoms and it’s not pleasant. It’s easy to think that ‘this won’t happen to me’ but it’s real and can be dangerous if ignored. On a day trip up to my local mountain, Mammoth Mountain, I ascended from around sea level to 11,053ft in just over 6 hours and I started feeling really tired and light-headed. I didn’t think much of it until I passed out on Chair 23. I’m just lucky I wasn’t actually riding at the time. I immediately descended to around 8,000ft, where I waited for the headache to subside. I finished the day out with very light riding below 9,500ft and ended up being okay.
Works Cited
[1] “National Aeronautics and Space Administration.” NASA, 2000, NASA.gov.
[2] Khan, April. “Altitude Sickness.” Healthline, Healthline Media, 16 Aug. 2012, www.healthline.com/health/altitude-sickness.
[3] Fuehrer, Justin, and Martin R. Huecker. “High Altitude Cardiopulmonary Diseases.” PubMed, StatPearls Publishing, 2020, www.ncbi.nlm.nih.gov/books/NBK442011/. Accessed 13 Jun. 2022.
[4] Nehring, Sara M, et al. “Cerebral Edema.” Nih.gov, StatPearls Publishing, 25 Mar. 2019, www.ncbi.nlm.nih.gov/books/NBK537272/.
[5] NHS Choices. “Altitude Sickness.” Altitude Sickness, 2019, www.nhs.uk/conditions/altitude-sickness/.
[6] Cleveland Clinic. “Altitude Sickness: Symptoms, Diagnosis, Treatment & Prevention.” Cleveland Clinic, 23 Sept. 2020, my.clevelandclinic.org/health/diseases/15111-altitude-sickness.
[7] “High-Altitude Pulmonary Edema – an Overview | ScienceDirect Topics.” Www.sciencedirect.com, www.sciencedirect.com/topics/medicine-and-dentistry/high-altitude-pulmonary-edema. Accessed 12 June 2022.